Written by doctor Mr. Stavros Athanasiou
What is a hysterectomy
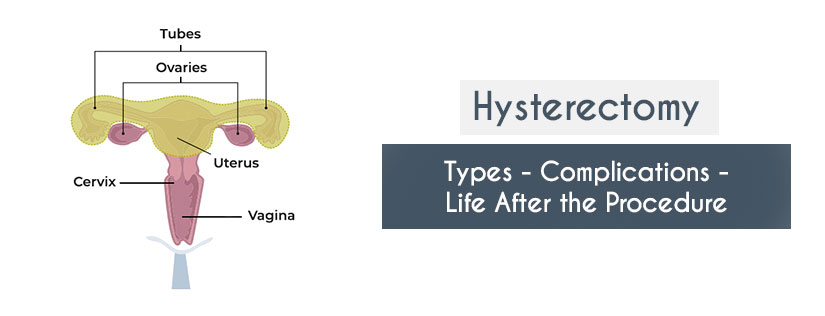
Hysterectomy is the surgical removal of the uterus. The entire uterus is usually removed during surgery. The doctor may also remove part of the fallopian tubes and ovaries, depending on the reason for the hysterectomy.
Why do I need a hysterectomy
-Uterine fibroids: Fibromyomas are non-cancerous tumors of the uterine wall. In some women, they can cause pain or heavy bleeding.
-Intense or unusual bleeding: Hormonal dysfunction,, infections, cancer or fibroids can cause persistent and heavy bleeding.
-Uterine prolapse: Uterine prolapse occurs when the uterus “drops” from its physiological anatomic position into the vagina. This is common in women who have had several vaginal deliveries but can also occur in menopausal women due to the weakening of the muscles or even due to obesity. For detailed information on uterine prolapse, click here.
-Endometriosis: Endometriosis occurs when the endometrial tissue (the lining that normally covers the inside wall of the uterus) grows outside the uterus and onto the ovaries. This can cause severe pain or bleeding at times.
-Adenomyosis: In this condition, part of the endometrial tissue (the lining that normally covers the inside wall of the uterus) penetrates and grows inside the muscular wall of the uterus. The displaced tissue continues to act normally — thickening, breaking down and bleeding — during each menstrual cycle, which can cause severe pain and bleeding.
-Cancer of the uterus, ovaries or endometrium: Hysterectomy is probably the best option when treating any of these cancers (e.g. cervical cancer). Other treatments may include chemotherapy or radiation therapy. In any case, you should consult your doctor.
Keep in mind that there are alternative ways to deal with any of the above problems that may not include a hysterectomy. However, hysterectomy is a major surgery, and you should talk to your doctor about the options you have for treating each of the above symptoms.
According to official statistics, about 23,000 women in Greece undergo a hysterectomy every year.
Will the doctor remove the ovaries during the hysterectomy?
Whether or not the ovaries are removed during a hysterectomy depends on the initial diagnosis.
The ovaries can be removed (oophorectomy) to reduce the risk of ovarian cancer. However, in premenopausal women an oophorectomy might lose the protective role estrogens have for conditions such as heart attacks or bone diseases (e.g. osteoporosis.)
Recent studies suggest removing the fallopian tubes (salpingectomy) and not the ovaries might reduce the risk of future ovarian cancer, as this is is thought to start in the fallopian tubes.
Deciding whether to keep or remove the ovaries is a decision you can make by discussing the risks and benefits of either choice with your doctor.
Will I become menopausal after the hysterectomy?
All premenopausal women who undergo a hysterectomy will stop menstruating. Whether you will have other menopausal symptoms after a hysterectomy depends on the preservation or not of the ovaries during surgery.
If you do not remove the ovaries, you will probably not have any menopausal symptoms but because the uterus is removed, you can no longer menstruate and therefore become pregnant.
If both ovaries are removed during a hysterectomy, you will no longer menstruate and may immediately experience menopausal symptoms. As your hormone levels drop quickly, the symptoms can be much more intense than in the case of normal-age menopause.
Consult your doctor for methods of treating these symptoms.
How is a hysterectomy performed?
Hysterectomy can be done in many different ways. It depends on your medical history and the reason you have the surgery.
– Abdominal hysterectomy: The doctor usually makes an incision in the lower abdomen. It is usually done in cases of cervical, uterine or ovarian cancer. The disadvantage of abdominal hysterectomy is that it can be quite painful.
– Transvaginal hysterectomy: It is performed through a small incision in the vagina. This method will not leave a visible wound or scar and is usually performed for benign conditions. It is the preferred approach for uterine prolapse. The procedure can be performed under regional or even local anaesthesia without the need for general anaesthetic and is associated has the advantage of fast recovery.
– Laparoscopic hysterectomy: It is performed with small incisions in the abdominal wall, and the uterus is removed from the vagina.
Does the operation have complications?
Some of the most common complications of hysterectomy include:
– Pelvic infections
– Bladder infections
– Menopause (in case of removal of the ovaries as already mentioned)
– Kidney infections
– Psychological effects
TRASNVAGINAL HYSTERECTOMY
– Faster recovery – Shorter recovery time
– Less painful method compared to abdominal hysterectomy
– Does not leave any scars on the abdomen
ABDOMINAL HYSTERECTOMY
– Longer recovery time than transvaginal hysterectomy
– A painful method
– Postoperative scars in the abdomen
Hysterectomy and alternative therapies
Sometimes a hysterectomy can be medically unavoidable, such as, e.g. in cases of prolonged bleeding or some cases of cancer. However, you can try other solutions first that may prevent the need for a hysterectomy. These include:
Kegel Excersices: In case of uterine prolapse, you can try Kegel exercises. Kegel exercises help restore the muscles that hold the uterus in place. Read more about Kegel exercises.
Medication: Your doctor may prescribe medication to help with endometriosis.
Vaginal pessary (in case of uterine prolapse). A vaginal pessary is a device inserted into the vagina and helps support the vaginal walls. There are different types of pessaries and, their shape is similar to the diaphragm. The vaginal pessary is inserted into the vagina to hold the uterus. Uterine prolapse occurs when the uterus falls due to loss of support after childbirth or pelvic surgery.
Surgery: You can always choose the surgical solution with smaller incisions in consultation with the doctor. The fewer and smaller incisions the surgery involves, the faster the wounds will heal, and you will return to regular activity. Depending on your symptoms, these solutions may include:
Alternative surgeries
– Surgery to treat endometriosis: Laparoscopic surgery using a small thin tube with a tiny camera. The surgeon inserts the camera and surgical instruments into the pelvic area through small incisions. You can still get pregnant after this surgery.
– Surgery to remove uterine fibroids without removing the uterus: This procedure is called a Myomectomy. It is the removal of fibroids while maintaining the uterus. Depending on the location of the fibroids, fibroids can be removed laparoscopically through the abdominal wall or hysteroscopically through the vagina and cervix. You can also get pregnant after this operation.
How common hysterectomy
Every year in the United States, about 630 thousand women undergo a hysterectomy. Hysterectomy is the second most common surgery in women in the US, while the most common surgery is a caesarean section during the birth process.
In Greece, according to official statistics, about 23 thousand women undergo a hysterectomy every year.
Types of hysterectomy
Total hysterectomy
In this case, the entire uterus is removed, along with the cervix. The ovaries and fallopian tubes may or may not be removed. It is the most common type of hysterectomy.
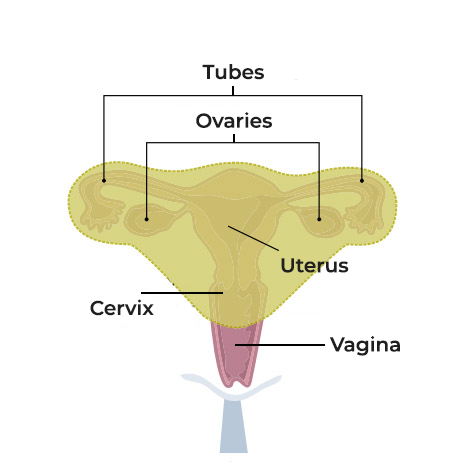
Subtotal Hysterectomy
In this case, the cervix remains in place. Also the ovaries can be removed or not.
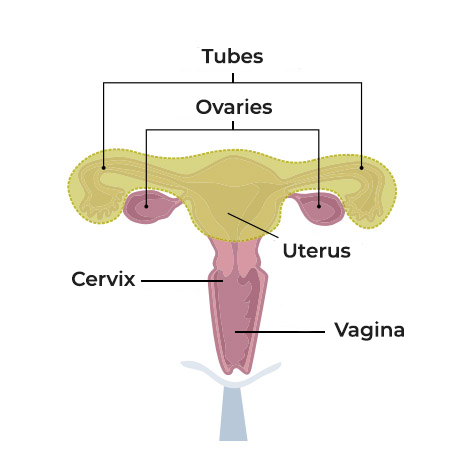
Radical Hysterectomy
The entire uterus, as well as the upper part of the vagina and some pelvic lymph nodes are removed. Radical hysterectomy is performed in certain types of cancer, such as cervical cancer. The fallopian tubes and ovaries may or may not be removed.
How long does recovery after a hysterectomy take?
Recovery after hysterectomy usually takes 4 to 6 weeks. Most women stay in the hospital for a day or two after surgery. However, some may last longer, especially when cancer is the underlying cause of the hysterectomy.
The time you need to return to normal activities depends on the type of surgery:
– Abdominal hysterectomy can take 4 to 6 weeks
– Vaginal or laparoscopic hysterectomy can take up to 3-4 weeks.
After the operation, rest is necessary, and you should avoid heavy lifting. During this period, which is usually 4 to 6 weeks, you should refrain from sexual intercourse as the incision in the vagina will not have healed and may cause pain.
What changes to expect after a hysterectomy
Hysterectomy is a serious operation, and so it may take a few weeks for you to heal (4 to 6 weeks as mentioned). However, for most women, it is a significant change in their lives. Other changes you will see are:
– You will not menstruate again
– Change in sexual life: Some women have vaginal dryness or low libido after a hysterectomy, especially if the ovaries are removed.
– Increased risk for other health problems: Removing both ovaries may increase the risk of certain diseases, such as heart attacks, osteoporosis and urinary incontinence. Talk to your doctor about how you can prevent these problems.
– Depression : Some women may experience depression due to loss of fertility or a change in their body.
Will I need any examination or tests after a hysterectomy?
– You will still need to have regular Pap tests if:
– The cervix has not been removed (That is if you have undergone a subtotal hysterectomy)
– You had a hysterectomy because of a cancerous tumor
– There is a history of lesions in the cervix
Contact our office to learn more about hysterectomy and to discuss with your doctor the case of hysterectomy.
Contact our office to learn more about hysterectomy and to discuss with your doctor the case of hysterectomy.